
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
- A Multicentre, Multinational, Open-Label, 52-Week Extension Study of Gemigliptin (LC15-0444) Monotherapy in Patients with Type 2 Diabetes Mellitus
- Sae Jeong Yang, Kyung Wan Min, Sandeep Kumar Gupta, Joong Yeol Park, Vyankatesh K.Shivane, Pankaj Kumar Agarwal, Doo Man Kim, Yong Seung Kim, Sei Hyun Baik
- Diabetes Metab J. 2021;45(4):606-612. Published online September 9, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0047
- 5,034 View
- 139 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
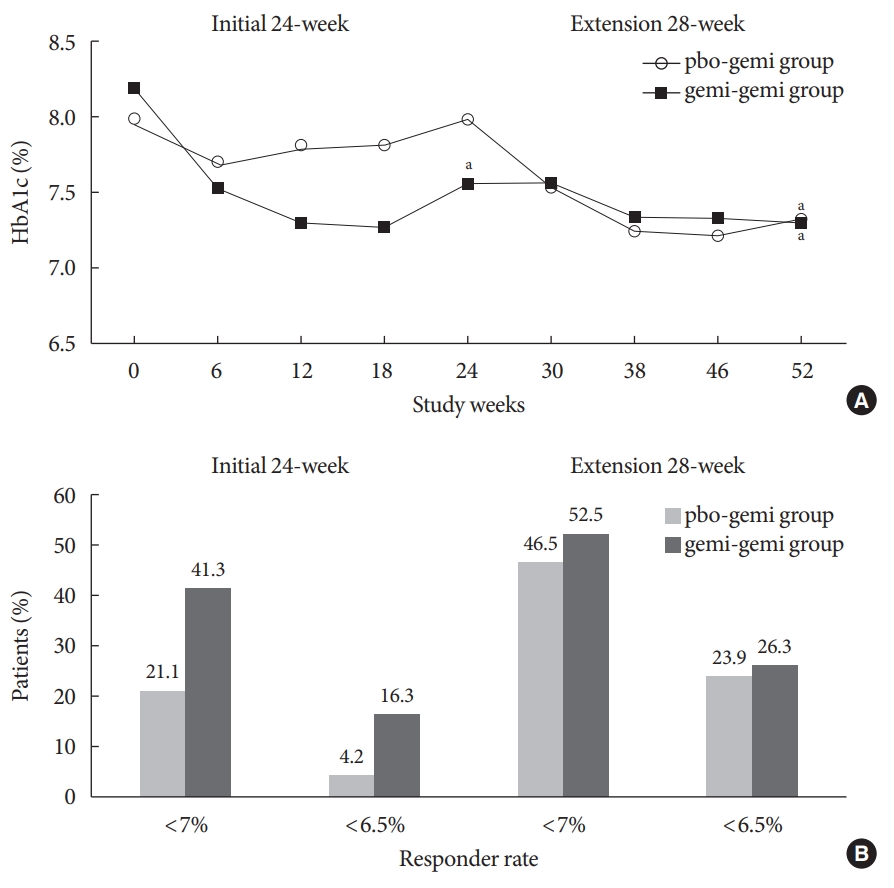
ePub - The purpose of this extension study was to assess the long-term efficacy and safety of gemigliptin 50 mg in patients with type 2 diabetes mellitus (T2DM). Patients with T2DM who had completed the initial 24-week study comparing gemigliptin monotherapy with placebo were eligible to enrol. In the open-label, 28-week extension study, all enrolled patients received gemigliptin, regardless of the treatment received during the initial 24-week study period. The mean reduction±standard deviation (SD) in glycosylated hemoglobin (HbA1c) observed after 24 weeks of treatment (–0.6%±1.1%) was further decreased for the gemi-gemi group and the mean change in HbA1c at week 52 from baseline was –0.9%±1.2% (P<0.0001). For the pbo-gemi group, HbA1c decreased after they were switched to gemigliptin, and the mean change in HbA1c at week 52 from baseline was –0.7%±1.2% (P<0.0001). Furthermore, the overall incidence of adverse events demonstrated that gemigliptin was safe and well tolerated up to 52 weeks.
-
Citations
Citations to this article as recorded by- Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef
- Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
- Clinical Diabetes & Therapeutics
- Efficacy and Safety of Voglibose Plus Metformin in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Trial
- Tae Jung Oh, Jae Myung Yu, Kyung Wan Min, Hyun Shik Son, Moon Kyu Lee, Kun Ho Yoon, Young Duk Song, Joong Yeol Park, In Kyung Jeong, Bong Soo Cha, Yong Seong Kim, Sei Hyun Baik, In Joo Kim, Doo Man Kim, Sung Rae Kim, Kwan Woo Lee, Jeong Hyung Park, In Kyu Lee, Tae Sun Park, Sung Hee Choi, Sung Woo Park
- Diabetes Metab J. 2019;43(3):276-286. Published online December 7, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0051
- 7,050 View
- 98 Download
- 13 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Combination of metformin to reduce the fasting plasma glucose level and an α-glucosidase inhibitor to decrease the postprandial glucose level is expected to generate a complementary effect. We compared the efficacy and safety of a fixed-dose combination of voglibose plus metformin (vogmet) with metformin monotherapy in drug-naïve newly-diagnosed type 2 diabetes mellitus.
Methods A total of 187 eligible patients aged 20 to 70 years, with a glycosylated hemoglobin (HbA1c) level of 7.0% to 11.0%, were randomized into either vogmet or metformin treatments for 24 weeks. A change in the HbA1c level from baseline was measured at week 24.
Results The reduction in the levels of HbA1c was −1.62%±0.07% in the vogmet group and −1.31%±0.07% in the metformin group (
P =0.003), and significantly more vogmet-treated patients achieved the target HbA1c levels of <6.5% (P =0.002) or <7% (P =0.039). Glycemic variability was also significantly improved with vogmet treatment, estimated by M-values (P =0.004). Gastrointestinal adverse events and hypoglycemia (%) were numerically lower in the vogmet-treated group. Moreover, a significant weight loss was observed with vogmet treatment compared with metformin (−1.63 kg vs. −0.86 kg,P =0.039).Conclusion Vogmet is a safe antihyperglycemic agent that controls blood glucose level effectively, yields weight loss, and is superior to metformin in terms of various key glycemic parameters without increasing the risk of hypoglycemia.
-
Citations
Citations to this article as recorded by- Phytochemical analysis and antihyperglycemic activity of Castilleja arvensis
Mónica Aideé Díaz-Román, Juan José Acevedo-Fernández, Gabriela Ávila-Villarreal, Elizabeth Negrete-León, A. Berenice Aguilar-Guadarrama
Fitoterapia.2024; 174: 105839. CrossRef - YAP/TAZ axis was involved in the effects of metformin on breast cancer
Yu Xu, Hongke Cai, Yuanfeng Xiong, Li Tang, Longjiang Li, Li Zhang, Yi Shen, Yongqiang Yang, Ling Lin, Jiayi Huang
Journal of Chemotherapy.2023; 35(7): 627. CrossRef - Diabetes remission: Myth or reality?
Ashok Kumar, ShubhaLaxmi Margekar, Ravi Kumar
Indian Journal of Medical Specialities.2023; 14(1): 3. CrossRef - Analysis of Reports Sent to the Portuguese Pharmacovigilance System and Published Literature Regarding the Safety of Metformin in the Elderly
Beatriz Esteves, Cristina Monteiro, Ana Paula Coelho Duarte
Healthcare.2023; 11(15): 2197. CrossRef - Rapid prediction method of α-Glycosidase inhibitory activity of Coreopsis tinctoria extract from different habitats by near infrared spectroscopy
Xiaogang He, Xiang Han, Jiaping Yu, Yulong Feng, Ganghui Chu
Spectrochimica Acta Part A: Molecular and Biomolecular Spectroscopy.2022; 268: 120601. CrossRef - Insulin autoimmune syndrome in patients with type 2 diabetes: A report of two cases
Y. Shin, T.J. Oh, S.H. Choi, H.C. Jang
Diabetes & Metabolism.2021; 47(1): 101115. CrossRef - Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Ki
Diabetes & Metabolism Journal.2021; 45(5): 675. CrossRef - Quantifying Remission Probability in Type 2 Diabetes Mellitus
Sanjay Kalra, Ganapathi Bantwal, Nitin Kapoor, Rakesh Sahay, Saptarshi Bhattacharya, Beatrice Anne, Raju A Gopal, Sunil Kota, Ashok Kumar, Ameya Joshi, Debmalya Sanyal, Mangesh Tiwaskar, Ashok Kumar Das
Clinics and Practice.2021; 11(4): 850. CrossRef - The effect of voglibose on metabolic profiles in patients with type 2 diabetes mellitus: A systematic review and meta-analysis of clinical trials
Peyman Nowrouzi-Sohrabi, Reza Tabrizi, Shahla Rezaei, Fatemeh Jafari, Kamran Hessami, Mehdi Abedi, Mohammad Jalali, Pedram Keshavarzi, Saeed Shahabi, Ali Asghar Kolahi, Kristin Carson-Chahhoud, Amirhossein Sahebkar, Saeid Safiri
Pharmacological Research.2020; 159: 104988. CrossRef - Role of Intestinal Microbiota in Metabolism of Voglibose In Vitro and In Vivo
Mahesh Raj Nepal, Mi Jeong Kang, Geon Ho Kim, Dong Ho Cha, Ju-Hyun Kim, Tae Cheon Jeong
Diabetes & Metabolism Journal.2020; 44(6): 908. CrossRef - Response: Efficacy and Safety of Voglibose Plus Metformin in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Trial (Diabetes metab J 2019;43;276-86)
Tae Jung Oh, Sung Hee Choi
Diabetes & Metabolism Journal.2019; 43(4): 547. CrossRef - Letter: Efficacy and Safety of Voglibose Plus Metformin in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Trial (Diabetes Metab J 2019;43;276-86)
Hannah Seok, Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(4): 545. CrossRef
- Phytochemical analysis and antihyperglycemic activity of Castilleja arvensis
- Perception of Clinicians and Diabetic Patients on the Importance of Postprandial Glucose Control and Diabetes Education Status: A Cross Sectional Survey
- Ji Hun Choi, Cheol Young Park, Bong Soo Cha, In Joo Kim, Tae Sun Park, Joong Yeol Park, Kyung Soo Park, Kun Ho Yoon, In Kyu Lee, Sung Woo Park
- Diabetes Metab J. 2012;36(2):120-127. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.120
- 3,854 View
- 33 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent studies have shown the importance of postprandial glucose (PPG) in the development of diabetes complications. This study was conducted in order to survey the perceptions of clinicians and diabetic patients with respect to PPG management and the current status of diabetes education.
Methods This was a cross-sectional study involving face-to-face interviews and an open questionnaire survey conducted in Korea. A total of 300 patients and 130 clinicians completed questionnaires, which included current education status, self monitoring of blood glucose (SMBG), criteria of diagnosis and management, and perceptions relating to PPG management.
Results While there was a significantly higher perceived need for diabetes education, the sufficiency of the current education was considered to be severely lacking. Fasting plasma glucose (FPG), PPG, and glycosylated hemoglobin (HbA1c) were all important considerations for clinicians when making a diagnosis of diabetes, although PPG was considered less important than FPG or HbA1c in the treatment of diabetes. Most clinicians and patients were aware of the importance of PPG, but actual education on the importance of PPG was not actively being delivered.
Conclusion Our study showed that the current status of diabetes education is insufficient to meet the needs of the Korean population. A considerable gap was found to exist between awareness and what was actually taught in the current education program in regard to the importance of PPG. These results suggest that clinicians need to be more active in patient education, especially in regard to the importance of PPG.
-
Citations
Citations to this article as recorded by- Addressing Overbasalization to Achieve Glycemic Targets
Kevin Cowart, Rachel Franks, Olivia Pane, Ellen Murphy, Kelly Oldziej
ADCES in Practice.2022; 10(2): 30. CrossRef - Post hoc efficacy and safety analysis of insulin glargine/lixisenatide fixed- ratio combination in North American patients compared with the rest of world
George Dailey, Harpreet S Bajaj, Terry Dex, Melanie Groleau, William Stager, Aaron Vinik
BMJ Open Diabetes Research & Care.2019; 7(1): e000581. CrossRef - Experiences of Diabetes Education among Educators of Diabetes : a content analysis approach
Soo Jin Kang, Soo Jung Chang
Journal of Korean Public Health Nursing.2016; 30(2): 221. CrossRef - Does Availability of Reliable Home Blood Glucose Data at Diabetes Appointments Improve Glycemia?
Gillian S. Boyd-Woschinko, David L. Kaiser, Michael Diefenbach, Ronald Tamler
Endocrine Practice.2014; 20(4): 299. CrossRef - Safety and effectiveness of insulin aspart in type 2 diabetic patients: Results from the ASEAN cohort of the A1chieve study
Wan Mohamad Wan Bebakar, Mary Anne Lim-Abrahan, Ananá B. Jain, Darren Seah, Pradana Soewondo
Diabetes Research and Clinical Practice.2013; 100: S17. CrossRef
- Addressing Overbasalization to Achieve Glycemic Targets
- Management of Blood Pressure in Patients with Type 2 Diabetes Mellitus: A Nationwide Survey in Korean
- Mi Hae Seo, Woo Je Lee, Cheol Young Park, Sung Rae Kim, Joong Yeol Park, Kun-Ho Yoon, Moon Kyu Lee, Sung Woo Park
- Diabetes Metab J. 2011;35(4):348-353. Published online August 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.4.348
- 3,829 View
- 33 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypertension is common in patients with type 2 diabetes, affecting up to 60% of patients. The Korean Diabetes Association performed a nationwide survey about prevalence, awareness and control of hypertension among diabetic Koreans.
Methods The current survey included 3,859 diabetic patients recruited from 43 hospitals in Korea. Age, gender, height, weight and blood pressure (BP) were measured by standard methods. Data on fasting plasma glucose, glycosylated hemoglobin (HbA1c), awareness of hypertension, and compliance of antihypertensive medication were collected via interview and reviewed using patient medical records.
Results A total of 57.5% of all patients were >60 years old. Their mean HbA1c was 7.6±1.5%. Among antihypertensive medication users, 39.9% had <130 mm Hg and <80 mm Hg, whereas 60.1% had ≥130 mm Hg or ≥80 mm Hg. The answer "BP is under good control" was given by 75.1% of the antihypertensive medication users. Out of these patients, 26.4% had <130 mm Hg and <80 mm Hg, whereas 73.6% had ≥130 mm Hg or ≥80 mm Hg. A total of 75.5% of antihypertensive medication users answered that they had taken their antihypertensive medication every day for the past 2 weeks. "Forgetfulness" was most frequently the reason of non-compliance for patients that did not take their antihypertensive medication regularly.
Conclusion Approximately one third of the patients with diabetes were found to reach target blood pressure control in the 43 hospitals across Korea. Stricter control is needed to reduce severe complications of diabetes in Korea.
-
Citations
Citations to this article as recorded by- Value of ambulatory blood pressure measurement in diagnosing hypotension in hypertensive diabetic patients with medication-controlled BP
Kamal Alghalayini
JRSM Cardiovascular Disease.2020; 9: 204800402093088. CrossRef - Association between blood pressure and target organ damage in patients with chronic kidney disease and hypertension: results of the APrODiTe study
Ran-hui Cha, Sejoong Kim, Sun Ae Yoon, Dong-Ryeol Ryu, Ji Eun Oh, Sang-Youb Han, Eun Young Lee, Dong Ki Kim, Yon Su Kim
Hypertension Research.2014; 37(2): 172. CrossRef - Blood Pressure Control According to the Prevalence of Diabetes in Renal Transplant Recipients
E. Zbroch, J. Malyszko, I. Glowinska, D. Maciorkowska, G. Kobus, M. Mysliwiec
Transplantation Proceedings.2013; 45(1): 200. CrossRef - Prevalence, awareness, treatment and control of hypertension in adults with diagnosed diabetes: The Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV)
H-S Lee, S-S Lee, I-Y Hwang, Y-J Park, S-H Yoon, K Han, J-W Son, S-H Ko, Y G Park, H W Yim, W-C Lee, Y-M Park
Journal of Human Hypertension.2013; 27(6): 381. CrossRef - Multi-Institutional Analysis of Localized Renal Cell Carcinoma that Demonstrates the Impact of Diabetic Status on Prognosis After Nephrectomy
Yun-Sok Ha, Won Tae Kim, Seok-Joong Yun, Sang-Cheol Lee, Wun-Jae Kim, Yong Hyun Park, Seok Ho Kang, Sung-Hoo Hong, Seok-Soo Byun, Yong-June Kim
Annals of Surgical Oncology.2013; 20(11): 3662. CrossRef
- Value of ambulatory blood pressure measurement in diagnosing hypotension in hypertensive diabetic patients with medication-controlled BP
- Regulation of Glucose Control in People with Type 2 Diabetes: A Review and Consensus
- Jeong-Taek Woo, Kyung Soo Park, Dong-Won Byun, Kyung Soo Ko, Yoon-Sok Chung, Doo Man Kim, Tae Sun Park, Bong Soo Cha, In Kyu Lee, Joong Yeol Park, Hyun Shik Son, Moon-Kyu Lee, Kwang Won Kim, Ho Young Son
- Korean Diabetes J. 2010;34(1):16-20. Published online February 28, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.1.16
- 3,365 View
- 47 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader A conference was convened by the Korean Diabetes Association and the Korean Endocrine Society on September 7, 2009 to discuss and organize the results of research on intensive glucose control for the prevention of cardiovascular disease in patients with type 2 diabetes. Professor Kyung Soo Park led the conference, and Professors Kwang Won Kim and Ho Young Son acted as chairmen. Professors Doo Man Kim, Tae Sun Park, and Bong Soo Cha reported on intensive glucose control and diabetic complications, including the UK Prospective Diabetes Study (UKPDS), Diabetes Control and Complication Trial (DCCT) research results, the recently published Action to Control Cardiovascular Risk in Diabetes (ACCORD), Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE), and Veterans Affairs Diabetes Trial (VADT) research, as well as meta-analyses. Professor Jeong-Taek Woo reported on the manuscript written by the committee for the Korean Diabetes Association which dealt with the treatment of diabetes mellitus. Professors Kyung Soo Ko, Joong Yeol Park, Hyun Shik Son, Moon-Kyu Lee, Dong-Won Byun, and Yoon-Sok Chung participated in the discussion and collected information for the manuscript from all of the participants. The aim of the debate was to determine how to establish target goals for intensive glucose control and how to individualize those goals. The participants concluded that there was no need to modify the recommendation of maintaining an HbA1c under 6.5%, the current blood glucose treatment goal that is recommended by the Korean Diabetes Association. In addition, individual target goals for glucose control were recommended depending on the situation of each patient. We report on the consensus statement from the meeting.
-
Citations
Citations to this article as recorded by- Long-term quality-of-care score for predicting the occurrence of acute myocardial infarction in patients with type 2 diabetes mellitus
Pi-I Li, How-Ran Guo
World Journal of Diabetes.2023; 14(7): 1091. CrossRef
- Long-term quality-of-care score for predicting the occurrence of acute myocardial infarction in patients with type 2 diabetes mellitus
- Frequency of Silent Myocardial Ischemia Detected by Thallium-201 SPECT in Patients with Type 2 Diabetes.
- Dong Woo Kim, Eun Hee Jung, Eun Hee Koh, Min Seon Kim, Joong Yeol Park, Seung Whan Lee, Seong Wook Park, Jin Sook Ryu, Ki Up Lee
- Korean Diabetes J. 2009;33(3):225-231. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.225
- 1,784 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Silent myocardial ischemia (SMI) is more common in diabetic patients than among the general population. It is not yet established whether a routine screening test for SMI is necessary, and which screening test would be most useful. The purpose of this study was to estimate the prevalence of SMI detected by Thallium-201 perfusion single photon emission computed tomography (SPECT) in type 2 diabetic patients. METHODS: A total of 173 asymptomatic type 2 diabetic patients were included in the study. Thallium-201 perfusion SPECT was performed to screen for SMI. RESULTS: Among the 173 patients, abnormal perfusion patterns were found in 11 patients. Coronary angiography was carried out for these patients, and significant coronary artery stenosis was found in ten of them (positive predictive value; 90.9%). There was a significant association between SMI and overt albuminuria (OR = 7.33, 95% CI, 1.825-29.437). CONCLUSION: Thallium-201 perfusion SPECT is not sensitive enough to identify SMI, but is accurate in detecting decreased myocardial perfusion. This may be a useful screening tool for detecting SMI in type 2 diabetic patients with impaired renal function.
- Nitric Oxide Increases Insulin Sensitivity in Skeletal Muscle by Improving Mitochondrial Function and Insulin Signaling.
- Woo Je Lee, Hyoun Sik Kim, Hye Sun Park, Mi Ok Kim, Mina Kim, Ji Young Yun, Eun Hee Kim, Sang Ah Lee, Seung Hun Lee, Eun Hee Koh, Joong Yeol Park, Ki Up Lee
- Korean Diabetes J. 2009;33(3):198-205. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.198
- 2,092 View
- 22 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Accumulating evidence has suggested that nitric oxide (NO) is involved in the regulation of insulin sensitivity in skeletal muscle. Recent studies also suggested NO as an important molecule regulating mitochondrial biogenesis. This study examined the effect of the NO donor, 3-morpholinosydnonimine (SIN-1), on glucose metabolism in skeletal muscle and tested the hypothesis that NO's effect on glucose metabolism is mediated by its effect on mitochondrial function. METHODS: In Sprague-Dawley (SD) rats treated with SIN-1 for 4 weeks, insulin sensitivity was measured by a glucose clamp study. Triglyceride content and fatty acid oxidation were measured in the skeletal muscle. In addition, mitochondrial DNA content and mRNA expression of mitochondrial biogenesis markers were assessed by real-time polymerase chain reaction and expression of insulin receptor substrate (IRS)-1 and Akt were examined by Western blot analysis in skeletal muscle. In C2C12 cells, insulin sensitivity was measured by 2-deoxyglucose uptake and Western blot analysis was used to examine the expression of IRS-1 and Akt. RESULTS: SIN-1 improved insulin sensitivity in C2C12 cells and skeletal muscles of SD rats. In addition, SIN-1 decreased triglyceride content and increased fatty acid oxidation in skeletal muscle. Mitochondrial DNA contents and biogenesis in the skeletal muscle were increased by SIN-1 treatment. Moreover, SIN-1 increased the expression of phosphor-IRS-1 and phosphor-Akt in the skeletal muscle and muscle cells. CONCLUSION: Our results suggest that NO mediates glucose uptake in skeletal muscle both in vitro and in vivo by improving mitochondrial function and stimulating insulin signaling pathways. -
Citations
Citations to this article as recorded by- NO-Rich Diet for Lifestyle-Related Diseases
Jun Kobayashi, Kazuo Ohtake, Hiroyuki Uchida
Nutrients.2015; 7(6): 4911. CrossRef - Metformin Activates AMP Kinase through Inhibition of AMP Deaminase
Jiangyong Ouyang, Rahulkumar A. Parakhia, Raymond S. Ochs
Journal of Biological Chemistry.2011; 286(1): 1. CrossRef
- NO-Rich Diet for Lifestyle-Related Diseases
- Anti-GAD Antibody in Patients with Adult-Onset Diabetes in Korea.
- Sang Ah Lee, Eui Young Kim, Eun Hee Kim, Ji Yun Jeong, Eun Heui Jeong, Dong Woo Kim, Eun Hee Cho, Eun Hee Koh, Min Seon Kim, Joong Yeol Park, Ki Up Lee
- Korean Diabetes J. 2009;33(1):16-23. Published online February 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.1.16
- 2,342 View
- 23 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It is well known that the clinical characteristics of diabetes mellitus in Korean people are different from those of Western people. The purpose of this study was to investigate the prevalence of the anti-GAD antibody (GADA) in a large number of Korean patients with adult-onset diabetes. METHODS: The GADA was measured by radioimmunoassay for 11,472 adult-onset diabetic patients who visited the Asan Medical Center from 1998 to 2007. According to the fasting C-peptide levels, we classified the patients into an insulin dependent diabetes mellitus group (IDDM; C-peptide < 0.6 ng/mL) and non-insulin dependent diabetes mellitus group (NIDDM; C-peptide > or = 1.0 ng/mL). Other clinical and laboratory data were obtained from medical records. RESULTS: Among the 11,147 diabetic patients, 9,250 patients were classified as NIDDM, 922 patients were classified as IDDM and 975 patients excluded. Within the latter group 472 patients were to absolute insulin deficient (C-peptide < 0.1 ng/mL). The prevalence of GADA was 22.0% in the IDDM group and 4.7% in the NIDDM group. GADA was more prevalent in younger-onset NIDDM patients (25~40 years of age; 12.4%) than in older-onset NIDDM patients (> or = 40 years of age; 3.8%). The GADA-positive NIDDM patients had lower C-peptide and BMI levels, and higher rates of typical diabetic symptoms and insulin treatment. CONCLUSION: The prevalence of GADA in Korean patients with IDDM and NIDDM was lower than that reported in Western populations. It is thus suggested that autoimmunity is a rarer cause of diabetes in Korean people. However, since over 10% of younger-onset NIDDM patients were positive for GADA, routine GADA measurement in such patients is recommended. -
Citations
Citations to this article as recorded by- Distinct changes to pancreatic volume rather than pancreatic autoantibody positivity: insights into immune checkpoint inhibitors induced diabetes mellitus
Hung-Hui Wei, Ying-Chieh Lai, Gigin Lin, Cheng-Wei Lin, Ya-Chu Chang, John Wen-Cheng Chang, Miaw-Jene Liou, I-Wen Chen
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - The effect of glargine versus glimepiride on pancreatic β-cell function in patients with type 2 diabetes uncontrolled on metformin monotherapy: open-label, randomized, controlled study
Jun Sung Moon, Kyoung Soo Ha, Ji Sung Yoon, Hyoung Woo Lee, Hyun Chul Lee, Kyu Chang Won
Acta Diabetologica.2014; 51(2): 277. CrossRef - Successful treatment of latent autoimmune diabetes in adults with Traditional Chinese Medicine: a case report
Jiaxing Tian, Wenke Liu, Zhong Zhen, Xiaolin Tong
Journal of Traditional Chinese Medicine.2013; 33(6): 766. CrossRef - The prevalence and characteristics of latent autoimmune diabetes in adults (LADA) and its relation with chronic complications in a clinical department of a university hospital in Korea
Mi-Oh Roh, Chan-Hee Jung, Bo-Yeon Kim, Ji-Oh Mok, Chul-Hee Kim
Acta Diabetologica.2013; 50(2): 129. CrossRef - Prevalence and Clinical Characteristics of Recently Diagnosed Type 2 Diabetes Patients with Positive Anti-Glutamic Acid Decarboxylase Antibody
Yul Hwangbo, Jin Taek Kim, Eun Ky Kim, Ah Reum Khang, Tae Jung Oh, Hak Chul Jang, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee, Young Min Cho
Diabetes & Metabolism Journal.2012; 36(2): 136. CrossRef - Body Composition Analysis in Newly Diagnosed Diabetic Adolescent Girls
Yong Hyuk Kim, Min Kyoung Song, Sochung Chung
Journal of Korean Society of Pediatric Endocrinology.2011; 16(3): 172. CrossRef - Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea
Jin Taek Kim, Tae Jung Oh, Ye An Lee, Jun Ho Bae, Hyo Jeong Kim, Hye Seung Jung, Young Min Cho, Kyong Soo Park, Soo Lim, Hak Chul Jang, Hong Kyu Lee
Diabetes & Metabolism Journal.2011; 35(2): 166. CrossRef - Progression to insulin deficiency in Korean patients with Type 2 diabetes mellitus positive for anti‐GAD antibody
S. A. Lee, W. J. Lee, E. H. Kim, J. H. Yu, C. H. Jung, E. H. Koh, M.‐S. Kim, J.‐Y. Park, K.‐U. Lee
Diabetic Medicine.2011; 28(3): 319. CrossRef - Anti-GAD Antibody in Patients with Adult-Onset Diabetes in Korea
Eun-Gyoung Hong
Korean Diabetes Journal.2009; 33(1): 13. CrossRef
- Distinct changes to pancreatic volume rather than pancreatic autoantibody positivity: insights into immune checkpoint inhibitors induced diabetes mellitus
- Retraction: Protective Effect of PGC-1 on Lipid Overload-induced Apoptosis in Vascular Endothelial Cell.
- Eun Hee Koh, Youn Mi Kim, Ha Jung Kim, Woo Je Lee, Jong Chul Won, Min Seon Kim, Ki Up Lee, Joong Yeol Park
- Korean Diabetes J. 2008;32(3):293-293. Published online June 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.3.293
- 1,615 View
- 20 Download
- Changes in the Prevalence of Metabolic Syndrome in a Rural Area of Korea Defined by Two Criteria, Revised National Cholesterol Education Program and International Diabetes Federation.
- Jong Chul Won, Joong Yeol Park, Kee Ho Song, Woo Je Lee, Eun Hee Koh, Il Sung Nam-Goong, Sung Min Han, Moo Song Lee, Min Seon Kim, Ki Up Lee
- Korean Diabetes J. 2007;31(3):284-292. Published online May 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.3.284
- 2,124 View
- 16 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The prevalence of obesity is increasing in Korea, including rural areas. We examined the changes in the prevalence of metabolic syndrome (MetS), defined by revised National Cholesterol Education Program (NCEP) or International Diabetes Federation (IDF) criteria, in a rural area of Korea during the past 6 years. METHODS: A total of 1,119 subjects (424 men and 695 women) aged > or = 30 years were initially recruited in 1997. Baseline clinical data and various laboratory values were obtained. Six years later, we performed a follow-up study in 814 subjects (316 men and 498 women) of which 558 were original participants and 256 subjects were new. The prevalence of MetS was assessed by the criteria of NCEP or IDF. RESULTS: The prevalence of central obesity and impaired fasting glucose increased in both sexes during the period between 1997 and 2003. The prevalence of MetS according to the IDF criteria also increased. In men, the age-adjusted prevalence of MetS was 10.9% in 1997 and 23.3% in 2003. In women, it was 42.2% in 1997 and 43.4% in 2003. However, the prevalence of MetS according to the NCEP criteria increased only in men. CONCLUSION: There have been increases in the prevalence of central obesity and MetS according to the IDF criteria during the recent 6 years in a rural area of Korea. -
Citations
Citations to this article as recorded by- The Association between Midnight Salivary Cortisol and Metabolic Syndrome in Korean Adults
Yun-Mi Jang, Eun Jung Lee, Dong Lim Kim, Suk Kyeong Kim, Kee-Ho Song
Diabetes & Metabolism Journal.2012; 36(3): 245. CrossRef - The Diagnostic Criteria of Metabolic Syndrome and the Risk of Coronary Heart Disease according to Definitions in Men
Hyouk-Soo Seo, Sung-Hi Kim, Soon-Woo Park, Jong-Yeon Kim, Geon-Ho Lee, Hye-Mi Lee
Korean Journal of Family Medicine.2010; 31(3): 198. CrossRef - Metabolic syndrome is associated with erosive esophagitis
Jung Ho Park, Dong IL Park, Hong Joo Kim, Yong Kyun Cho, Chong IL Sohn, Woo Kyu Jeon, Byung Ik Kim
World Journal of Gastroenterology.2008; 14(35): 5442. CrossRef
- The Association between Midnight Salivary Cortisol and Metabolic Syndrome in Korean Adults
- Protective Effect of PGC-1 on Lipid Overload-induced Apoptosis in Vascular Endothelial Cell.
- Eun Hee Koh, Youn Mi Kim, Ha Jung Kim, Woo Je Lee, Jong Chul Won, Min Seon Kim, Ki Up Lee, Joong Yeol Park
- Korean Diabetes J. 2006;30(3):151-160. Published online May 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.3.151
- 2,084 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Fatty acids contribute to endothelial cell dysfunction and apoptosis by inducing accumulation of long chain fatty acyl CoA (LCAC), which increases oxidative stress in vascular endothelial cells. Forced expression of PGC-1 was shown to induce mitochondrial biogenesis and to control expression of mitochondrial enzymes involved in fatty acid oxidation. This study was undertaken to test the hypothesis that PGC-1 overexpression could prevent endothelial cell apoptosis by enhancing fatty acid oxidation and relieving oxidative stress in vascular endothelium. METHODS: Adenoviruses containing human PGC-1 (Ad-PGC-1) and beta-galactosidase (Ad-beta-gal) were transfected to confluent human aortic endothelial cells (HAECs). To investigate the effect of adenoviral PGC-1 gene transfer on apoptosis, combined treatment of linoleic acid (LA), an unsaturated fatty acid, was performed. RESULTS: PGC-1 overexpression inhibited the increase in ROS production and apoptosis of HAECs induced by LA. Also, PGC-1 led to a significant increase in fatty acid oxidation and decrease in triglyceride content in HAECs. LA caused the decrease of adenine nucleotide translocase (ANT) activity and transient mitochondrial hyperpolarization, which was followed by depolarization. PGC-1 overexpression prevented these processes. CONCLUSION: In summary, PGC-1 overexpression inhibited mitochondrial dysfunction and apoptosis by facilitating fatty acid oxidation and protecting against the damage from oxidative stress in HAECs. The data collectively suggest that the regulation of intracellular PGC-1 expression might play a critical role in preventing atherosclerosis.
- Increase in Fatty Acid Oxidation by AICAR: the Role of p38 MAPK.
- Woo Je Lee, Jin Yob Kim, Sung Jin Bae, Eun Hee Koh, Sung Min Han, Hye Sun Park, Hyun Sik Kim, Min Seon Kim, Joong Yeol Park, Ki Up Lee
- Korean Diabetes J. 2005;29(1):15-21. Published online January 1, 2005
- 1,085 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
AMPK is an enzyme that increases glucose transport and fatty acid oxidation in skeletal muscle. The activation of AMPK stimulates fatty acid oxidation by decreasing the acetyl CoA carboxylase (ACC) activity and the concentration of malonyl-CoA. However, a recent study has reported a dissociation of AMPK activity and ACC phosphorylation in skeletal muscle during periods of prolonged exercise. This suggested that there is an additional mechanism for AMPK-induced fatty acid oxidation in skeletal muscle. METHODS: Plamitate oxidation was measured via the generation of [3H]-water generation from 9,10[3H]-palmitate after treating various concentrations of AICAR on the C2C12 mouse skeletal muscle cell line. Western analysis was used to test for the possible activation of p38 MAPK by AICAR. Involvement of p38 MAPK in the AICAR-induced increase in fatty acid oxidation was tested for by using SB203580, a p38 MAPK inhibitor. RESULTS: C2C12 cell treated with AICAR exhibited a dose-dependent increase in fatty acid oxidation compared to the cells that were not treated with AICAR. Western blot analysis revealed that phosphorylation of p38 MAPK was increased 2.5 folds after AICAR treatment. The increase of fatty acid oxidation with AICAR treatment was significantly inhibited by a treatment of SB203580; this indicated the involvement of p38 MAPK on the AICAR-induced increase in fatty acid oxidation. CONCLUSION: AICAR stimulated the fatty acid oxidation by activating p38 MAPK. This is a novel pathway by which AMPK activation in skeletal muscle increases the fatty acid oxidation
- AMPK Activator AICAR Inhibits Hepatic Gluconeogenesis and Fatty Acid Oxidation.
- Jin Yob Kim, Eun Hee Koh, Woo Je Lee, Seong Min Han, Ji Young Youn, Hye Sun Park, Hyun Sik Kim, Min Seon Kim, Joong Yeol Park, Ki Up Lee
- Korean Diabetes J. 2005;29(1):6-14. Published online January 1, 2005
- 1,207 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Recent studies have demonstrated that adiponectin and metformin activate AMPK in the liver, and adiponectin and metformin stimulate fatty acid oxidation while inhibiting glucose production in liver. These results are in contrast to previous studies that have demonstrated that increased fatty acid oxidation in the liver is associated with increased gluconeogenesis. The present study was undertaken to reinvestigate the effects of AMPK activation by AICAR on hepatic fatty acid oxidation and gluconeogenesis. METHODS: HePG2 cells were treated with various concentrations of AICAR, and then the fatty acid oxidation and gluconeogenesis of the cells were determined. To investigate the in vivo effect of AICAR, Sprague-Dawely rats were infused with AICAR (bolus, 40 mg/g; constant, 7.5 mg/g/min-1) for 90min. RESULTS: Incubation of the HePG2 cells with higher concentrations (=1 mM) of AICAR increased fatty acid oxidation and gluconeogenesis. On the other hand, incubation of HePG2 cells with lower concentrations (0.05 and 0.1 mM) of AICAR decreased fatty acid oxidation and gluconeogenesis. Consistent with this in vitro data, the intravenous administration of AICAR to rats lowered their plasma glucose concentration and inhibited hepatic gluconeogenesis. Fatty acid oxidation in the liver tissue was significantly decreased by the administration of AICAR. CONCLUSION: The present study has demonstrated that AICAR decreased gluconeo-genesis in the liver. In contrast to previous studies, AICAR profoundly decreased hepatic fatty acid oxidation in rats and also in cultured hepatocytes
- The Role of AMPK in Vascular Endothelium.
- Woo Je Lee, Jin Yob Kim, Eun Hee Koh, Sung Min Han, Min Seon Kim, Ki Up Lee, Joong Yeol Park
- Korean Diabetes J. 2005;29(1):1-5. Published online January 1, 2005
- 934 View
- 16 Download
- Hypothalamic AMPK Activity in Diabetic Rats.
- Churl Namkoong, Min Seon Kim, Woo Je Lee, Pil Geum Jang, Seong Min Han, Eun Hee Koh, Joong Yeol Park, Ki Up Lee
- Korean Diabetes J. 2004;28(6):468-477. Published online December 1, 2004
- 929 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
AMP-activated protein kinase (AMPK) acts as a cellular energy sensor that is activated during states of low energy charge and it regulates the various metabolic pathways to reestablish the normal cellular energy balance. It has recently been demonstrated that AMPK activity is altered by the state of energy metabolism in the hypothalamic neurons and this mediates the feeding response. METHODS: Diabetes was induced by an intra-peritoneal injection of streptozotocin (STZ) in Sprague-Dawley rats. The diabetic rats were maintained for 3 weeks with or without insulin treatment. 3 weeks later, we collected hypothalamus and we then assayed the phosphorylation of AMPK and the activity of acetyl CoA carboxylase (ACC) and isoform-specfic AMPK. To determine the effect of hypothalamic AMPK inhibition on diabetic hyperphagia, we administered an AMPK inhibitor, compound C, into the third ventricle in the STZ-induced diabetic rats. RESULTS: Phosphorylation of AMPK, which is a marker of AMPK activation, increased in the hypothalamus of the STZ-induced diabetic rats (DR). Moreover, 2-AMPK activity, but not 1-AMPK activity, increased by 2-fold in hypothalamus of the DRs. Phosphorylation of hypothalamic acetyl CoA carboxylase (ACC), a key downstream enzyme of AMPK, also increased in the DRs and this caused a reduction in ACC activity. Insulin treatment completely reversed the diabetesinduced changes in the hypothalamic AMPK and ACC, suggesting that insulin deficiency was associated with the changes in hypothalamic AMPK and ACC. Inhibition of AMPK by an intracerebroventricular administration of AMPK inhibitor, compound C, attenuated the development of diabetic hyperphagia and reduced the blood glucose levels in DRs. CONCLUSION: We have demonstrated that hypothalamic AMPK activity increased in the DRs, and inhibition of hypothalamic AMPK activity attenuated the development of diabetic hyperphagia. These data indicate that the enhanced hypothalamic AMPK activity may contribute to the development of diabetic hyperphagia

 KDA
KDA
 First
First Prev
Prev





